Patients will see direct benefits from a new agreement connecting physicians with university researchers in northern Colorado.
Joint research at Colorado State University, Poudre Valley Hospital and the Medical Center of the Rockies already has spawned development of several medical improvements, including a new arterial stent that helps prevent blood clotting and a hernia patch that fights infection.
Now, as part of a newly signed memorandum of understanding, the organizations have agreed to combine resources and personnel to bring CSU research to patients faster and more efficiently. The entities will collaborate in several areas, including clinical trials, funding opportunities, technology transfer, employee education/training and marketing.
“We’re translating academic research into real-world solutions,” said Melissa Reynolds, an associate professor of chemistry at CSU who is collaborating with local physicians on products that promote healing. “We get to have discussions about what the actual needs are at the clinical level. And that’s a value that can’t be replaced by anything else.”
Dr. Gary Luckasen, medical director of research at the Medical Center of the Rockies in Loveland and a CSU alumnus, added that the agreement promotes new partnerships between CSU and the two hospitals’ parent organization, University of Colorado Health.
Luckasen said that the organizations need each other: The hospitals rely on the research that is done at CSU, whether it be with animals or in a chemistry lab, and CSU requires access to the doctors and human patients who will use the products and treatments that emerge from the research.
More funding opportunities

Reynolds said the agreement improves the entities’ chances of landing research grants, since funding agencies look more favorably on existing collaborations than proposals for creating new partnerships from scratch. Having to draw new agreements and non-disclosure arrangements for each collaborative project creates delays, she said, so the partnership also streamlines and speeds the process for launching and funding new initiatives.
“It really breaks down a lot of barriers to interdisciplinary and translational research,” Reynolds said. “When you bring this group together, you break down the obstacles and merge the academics with the clinical side. It benefits students, too, because they’ll have access to the end users of what their research is focused on.”
She added that too often research ends at the academic level because there is no connection to real-world applications and manufacturing. The new agreement allows CSU faculty to work alongside doctors and understand their needs while developing realistic solutions that will be cost-effective in the marketplace.
“Does the chemistry and engineering get us all the way to the bedside?” Reynolds asked. “If it costs the consumer 100 times more, that isn’t going to happen.”
Dr. Julie Dunn, medical director of trauma research and education at the Medical Center of the Rockies, started collaborating with Reynolds after the two met in August 2012. They were at a gathering organized by CSU Professor Stuart Tobet, director of the School of Biomedical Engineering, to discuss unmet medical needs and ways that CSU researchers might help meet those needs. It was also at that meeting where Dunn met Jennifer Mueller, a professor of mathematics and biomedical engineering at CSU. Together, they are now studying the effectiveness of a new non-invasive method of monitoring lung function in real time using electrical impulses measured on the skin, without the need for radiation and dye. They are conducting a study on the technology, called electrical impedance tomography, in the intensive care unit at MCR.
The agreement
The agreement will give the hospitals and CSU access to each other’s clinical trials, and hospital physicians will be able to act as co-investigators for sponsored research at the university.
The initial areas targeted for research are cancer, cardiovascular disease, infectious disease, diabetes and metabolic disease, neuroscience, sports medicine, and women’s health issues
The entities also will engage in joint marketing, business development and research funding opportunities.
The agreement also calls for improving and increasing funding and peer-reviewed publications by sharing “complementary knowledge, skill sets, laboratories, equipment and other applicable resources” as well as providing joint seminar/lecture opportunities or even an annual research symposium.
Under a separate agreement, CSU’s tech transfer and commercialization entity CSU Ventures will provide service, training and assistance to the hospitals.
Kevin Unger, president and CEO of Poudre Valley Hospital and Medical Center of the Rockies, said the agreement is a step forward in the progression of a long-standing relationship between the hospitals and university.
“Northern Colorado and, for that matter, the nation have greatly benefited from research projects that we and CSU have done together over the years,” he said. “Our fruitful collaboration has enhanced the quality of care for our patients while helping CSU continue to be successful with its research.”
“CSU has a longstanding commitment — crossing many disciplines and academic colleges — to transformational research that advances our understanding of human health and well-being,” said CSU President Tony Frank. “This agreement builds on that strength, laying the groundwork for important advances in treatment and patient care. We’re proud of what we’ll be able to achieve and grateful to Kevin Unger for his willingness to explore new ways for us to work together to serve our community.”
CSU and the hospitals are already working together on several projects:
A new hernia patch
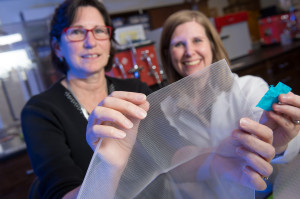
Reynolds is working with Dunn and two CSU faculty members in the Department of Microbiology, Immunology and Pathology, Brad Borlee and Richard Bowen, to develop a new mesh patch for hernia treatment.
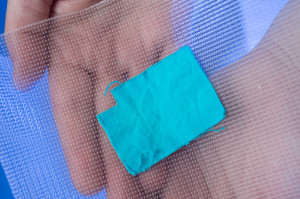
Traditional mesh patches used to close, secure and heal ruptures and swelling inside the body known as hernias are generally effective but can have severe side effects. Existing patches can cause infection and can invoke the body’s immune response to foreign substances and be rejected. They also don’t promote healing, because they can inhibit the natural, progressive growth of cell layers over the wound. Unlike a Band-Aid, Reynolds said, both sides of an internal hernia patch matter: It has to be antibacterial on the side that touches the rupture and receptive to the layers of tissue that should grow on the outside to heal it.
Reynolds and her team have developed a substance that can be sprayed onto Dunn’s favorite mesh patches and prompt chemical cues that cause the right cells to grow at the right times in the right places. The timed release of the chemical reactions discourages the growth of bacteria and the wrong type of cells, while promoting the development of cell layers that cover each other in the proper order.
Reynolds stressed that this effort and the other joint projects between CSU and the hospital system require a multidisciplinary approach involving various university departments.
“It’s not a magic bullet,” she said. “We are harnessing a variety of materials into one surface. We’re not experts in everything. We need multiple perspectives if we’re going to solve these grand challenges in the clinical arena.”
Improving the stent
Reynolds is also working with Luckasen and two CSU faculty members in the College of Engineering, Matthew Kipper and Ketul Popat, to develop a new stent for blood vessels.
Stents are tiny tubes that are inserted into blood vessels and act as a framework for keeping vessels open and blood flowing. The problem, Reynolds says, is that like chicken wire, stents have tiny holes in them that allow cells to grow into the middle of the tube and block blood flow, a condition called restenosis.
The CSU faculty are working with Luckasen to develop a new stent surface that better mimics the topography and chemical signaling of blood vessel walls, minimizing the body’s reaction to the foreign substance and keeping that extra cell growth out of the inner pathway.
Each of the three CSU faculty is contributing his or her particular expertise to a component of the project: Popat specializes in developing metal nanotubes, Kipper has developed an artificial sugar surface that mimics the outside of a cell, and Reynolds is providing a nitric oxide component to the surface, all of which combine to reduce clotting and restenosis.
“How do you make an artificial stent act like healthy blood vessels?” Reynolds said. “That’s what we’re trying to do.”
Luckasen said the hope is that the new stent will help prevent heart attacks without the need for blood thinners.
The goal is to conduct a clinical trial once the stent is developed.
Heart disease prevention
For nearly 15 years, hospital cardiologists — including Luckasen — have come to CSU’s Human Performance Clinical/Research Lab to supervise treadmill tests administered as part of the Heart Disease Prevention Program and interpret the results.
“What’s beneficial to us is if we have an abnormal test we can send the person to Poudre Valley Hospital quickly and easily,” said Tiffany Lipsey, who directs the program. “It is also helpful to have the cardiologist visit with the clients at the time of their test.”
The majority of those tested are firefighters, and in at least one case the relationship between CSU and the hospital had major implications. A Breckenridge firefighter who had an abnormal test was going to have to wait three months for an appointment at a clinic in Vail, meaning 90 days without pay during his medical hold. Lipsey said a Poudre Valley Hospital doctor was able to see him within a few days, and the firefighter had bypass surgery at the hospital the following week.
Poudre Valley Hospital’s Clinical Laboratory Services also does the bloodwork analysis for participants in the program. The hospital cardiologist also handles invasive procedures for the Human Cardiovascular Physiology Laboratory, which conducts research on understanding how blood vessels are controlled in humans.
Gay Israel, executive director of the Human Performance Clinical/Research Lab, said Luckasen supported the creation of the Heart Disease Prevention Program and provided cardiology services free of charge for many years.
“He’s been involved with this department for 30 years,” Israel said. “He’s a generous CSU alum and donor whose unwavering dedication has helped us make great strides.”
Media Assets
Video
High-Resolution Photos

Gary Luckasen, Melissa Reynolds and Julie Dunn in Reynolds’ laboratory at CSU.

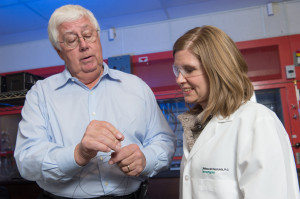
Dr. Gary Luckasen, left, and CSU Associate Professor Melissa Reynolds discuss the new stent they are developing.

Reynolds is applying a blue coating to enhance the mesh patch that Dr. Julie Dunn uses to repair hernias.

Megan Neufeld, one of Melissa Reynolds’ Ph.D. students in chemistry, works in the lab.

Dunn, left, and Reynolds show off the mesh material that is being treated to prevent infection and promote healing.